From University of California – San Diego 18/03/24
Our nervous systems are naturally wired to sense fear.
Whether prompted by the eerie noises we hear alone in the dark or the approaching growl of a threatening animal, our fear response is a survival mechanism that tells us to remain alert and avoid dangerous situations.
But if fear arises in the absence of tangible threats, it can be harmful to our well-being.
Those who have suffered episodes of severe or life-threatening stress can later experience intense feelings of fear, even during situations that lack a real threat.
Experiencing this generalization of fear is psychologically damaging and can result in debilitating long-term mental health conditions such as post-traumatic stress disorder (PTSD).
The stress-induced mechanisms that cause our brain to produce feelings of fear in the absence of threats have been mostly a mystery.
Now, neurobiologists at the University of California San Diego have identified the changes in brain biochemistry and mapped the neural circuitry that cause such a generalized fear experience.
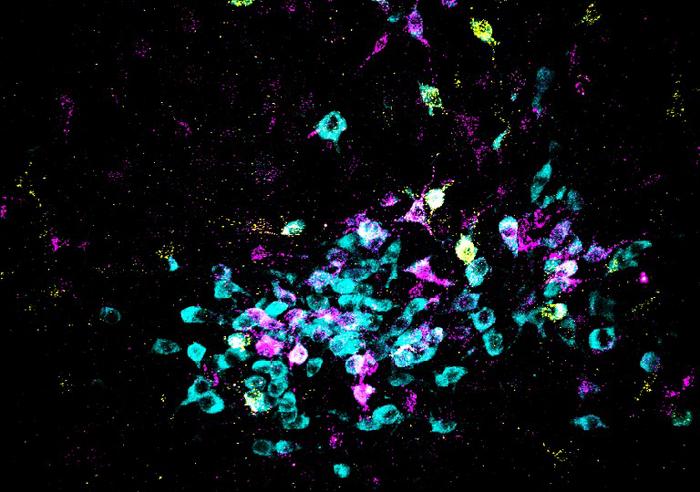
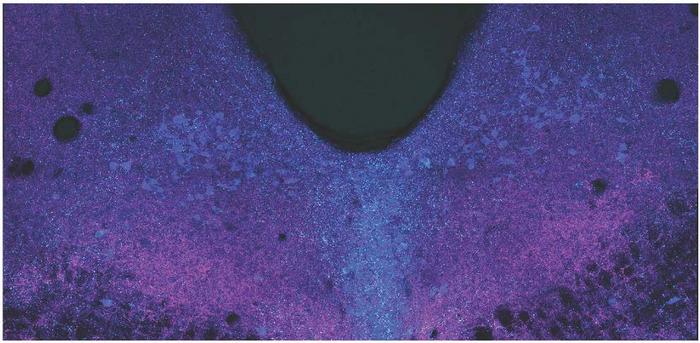
Spitzer Lab, UC San Diego
Their research, published in the journal Science on March 15, 2024, provides new insights into how fear responses could be prevented.
In their report, former UC San Diego Assistant Project Scientist Hui-quan Li, (now a senior scientist at Neurocrine Biosciences), Atkinson Family Distinguished Professor Nick Spitzer of the School of Biological Sciences and their colleagues describe the research behind their discovery of the neurotransmitters — the chemical messengers that allow the brain’s neurons to communicate with one another — at the root of stress-induced generalized fear.
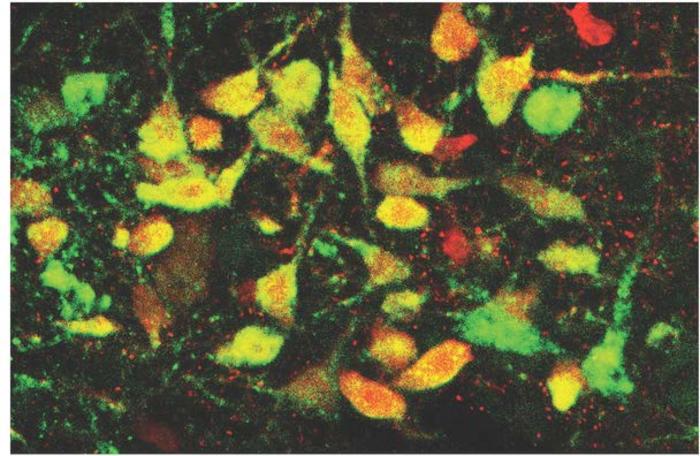
Studying the brains of mice in an area known as the dorsal raphe (located in the brainstem), the researchers found that acute stress induced a switch in the chemical signals in the neurons, flipping from excitatory “glutamate” to inhibitory “GABA” neurotransmitters, which led to generalized fear responses.
“Our results provide important insights into the mechanisms involved in fear generalization,” said Spitzer, a member of UC San Diego’s Department of Neurobiology and Kavli Institute for Brain and Mind.
“The benefit of understanding these processes at this level of molecular detail — what is going on and where it’s going on — allows an intervention that is specific to the mechanism that drives related disorders.”
Building upon this new finding of a stress-induced switch in neurotransmitters, considered a form of brain plasticity, the researchers then examined the postmortem human brains of individuals who had suffered from PTSD.
A similar glutamate-to-GABA neurotransmitter switch was confirmed in their brains as well.
The researchers next found a way to stop the production of generalized fear.
Prior to the experience of acute stress, they injected the dorsal raphe of the mice with an adeno-associated virus (AAV) to suppress the gene responsible for synthesis of GABA.
This method prevented the mice from acquiring generalized fear.
Further, when mice were treated with the antidepressant fluoxetine (branded as Prozac) immediately after a stressful event, the transmitter switch and subsequent onset of generalized fear were prevented.
Not only did the researchers identify the location of the neurons that switched their transmitter, but they demonstrated the connections of these neurons to the central amygdala and lateral hypothalamus, brain regions that were previously linked to the generation of other fear responses.
“Now that we have a handle on the core of the mechanism by which stress-induced fear happens and the circuitry that implements this fear, interventions can be targeted and specific,” said Spitzer.