From International Association for the Study of Lung Cancer 13/09/23

Identifying and analyzing volatile organic compounds in exhaled breath of patients with malignant pleural mesothelioma showed promise as a screening method for MPM, according to research presented today at the International Association for the Study of Lung Cancer (IASLC) 2023 World Conference on Lung Cancer in Singapore.
Malignant pleural mesothelioma (MPM) is a challenging disease with limited treatment options and a poor prognosis.
To improve treatment outcomes and tailor therapies for individual patients, researchers have been exploring predictive markers.
Recently, volatile organic compounds (VOCs) in exhaled breath have emerged as potential non-invasive markers for disease.

Kevin Lamote, PhD, from the University of Antwerp, Belgium, and colleagues conducted a study aimed to investigate whether exhaled breath analysis could differentiate treatment responders from non-responders (discriminative setup) and, if successful, predict treatment outcomes earlier (predictive setup) using VOCs as predictive biomarkers.
Dr. Lamote and his team examined 13 patients with MPM and subjected them to a CT scan before and every three months after treatment, with treatment responses scored as stable (SD) or progressive (PD) based on mRECIST criteria.
Breath and background samples were collected from the patients at each time point using multi-capillary column-ion mobility spectrometry (MCC-IMS) to characterize VOCs.
A lasso regression was performed to identify VOCs that could differentiate between responders and non-responders after treatment.
Additionally, a predictive model was trained to forecast treatment outcomes based on associated breath samples from previous study visits.
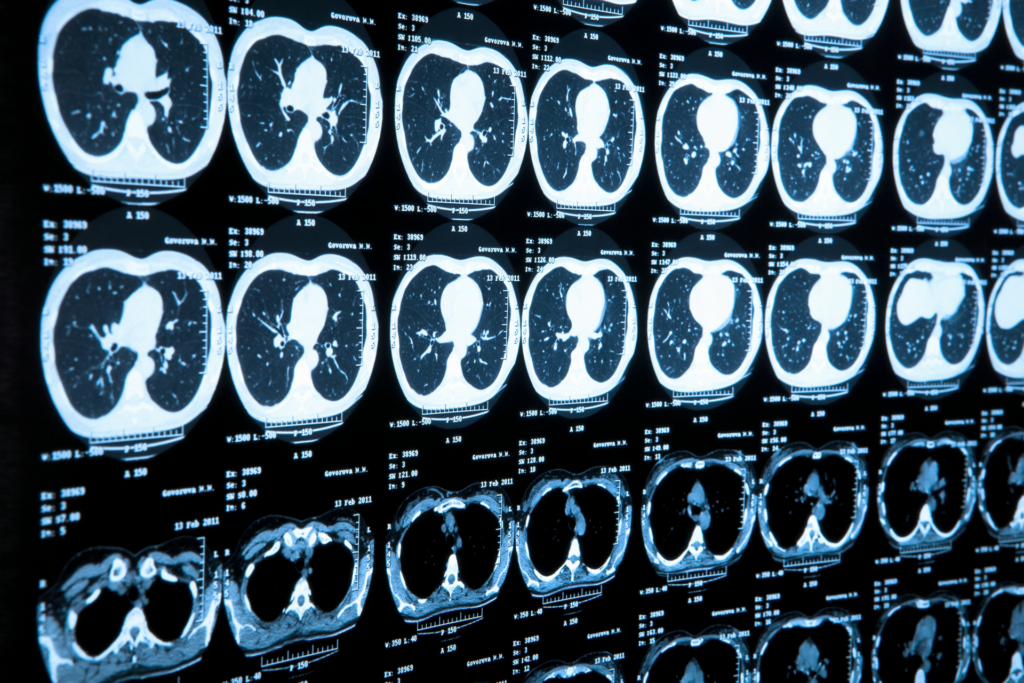
The study demonstrated an 89% accuracy (95% CI: 67.9-98.1) in distinguishing between SD and PD patients during follow-up.
Equally promising, the predictive model achieved the same level of accuracy at baseline in predicting treatment outcomes.
Notably, there were no significant differences in treatment approaches between SD and PD patients, suggesting that the selected VOCs may be involved in general mechanisms or correlated with the tumor microenvironment rather than being treatment-specific.
“The identification of VOCs in exhaled breath represents a promising opportunity for non-invasive detection and prediction of treatment outcomes in MPM patients,” said Dr. Lamote.
“However, to further validate the utility of the VOC profile, larger population studies are required.”
“Fine-tuning the VOC profile for each treatment could also help predict which patients are most likely to benefit from specific therapies, ultimately leading to improved overall treatment regimens for MPM.”